Explore the information below for helpful details about your digital ID card, provider networks, and additional plan resources.

Understanding Your ID Card
To support Whole Foods Market's commitment to the environment, the Whole Health Plan utilizes digital ID cards. Individual covered members each have a unique digital ID card. Enrolled Team Members have access to digital ID cards for dependent children under age 18; spouses or dependents over age 18 will need to create their own account to access their digital ID card.
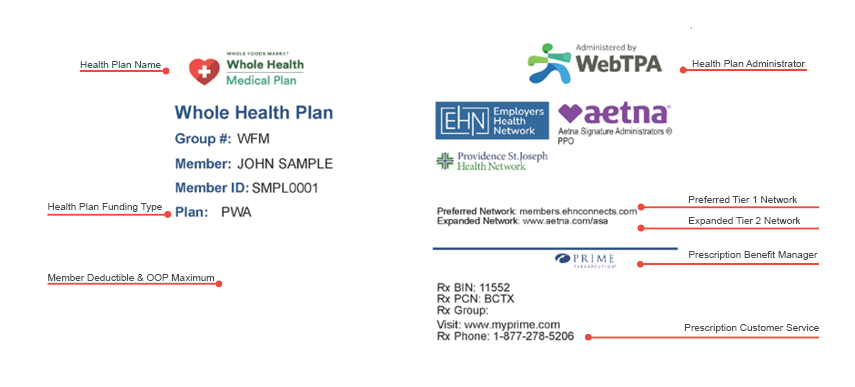
Below is a breakdown of a sample Whole Health Plan ID card. Your digital ID card can be found on your Member Portal.
Provider Networks & Plan Resources
Preferred Network
The Preferred Network is managed by Employers Health Network. The Preferred Network is a curated network of recognized local providers, clinics, and hospitals that have partnered with Whole Foods Market. These services are offered at a significantly lower deductible and out-of-pocket maximum when compared to the Expanded Network.
How do I find a Preferred Network Provider?
To find a Preferred Network Provider, log in to your Member Portal and utilize the Find a Provider search tool.
Questions?
Call 844-380-4554 to speak with a Health Resource Coordinator.
Expanded Network
The Expanded Network is managed by Aetna Signature Administrators. The Expanded Network is a national network of providers, clinics, and hospitals through Aetna Signature Administrators. Receiving care in this Expanded Network results in a significantly higher deductible and out-of-pocket maximum than the Preferred Network.
How do I find an Expanded Network Provider?
To find an Expanded Network Provider, log in to your Member Portal and utilize the Find a Provider search tool.
Questions?
Call 844-380-4554 to speak with a Health Resource Coordinator.
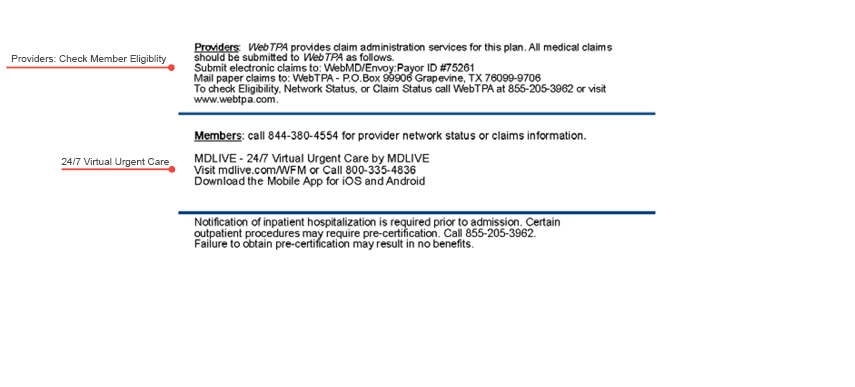
Log in to your Member Portal to find an in-network provider and utilize the Find a Provider search tool for cost estimates. All claims are administered by WebTPA, regardless of the network you are accessing. Submit all claims to WebTPA using the instructions on the back of your digital ID card.
Prescription Benefits Manager
Whole Health Plan prescription benefits are managed by Prime Therapeutics. Whole Health Plan participants automatically receive in-network prescription drug coverage through Prime Therapeutics.
How do I find an in-network pharmacy?
To find an in-network pharmacy, log in to your Prime Therapeutics Member Portal
Questions?
Call 1-877-278-5206 to speak with Prime Therapeutics Member Service.
Concierge Health Resource Coordination
The Whole Health Care Team provides Team Members with a single point of contact to help navigate treatment plans and maximize your benefits. A Health Resource Coordinator will provide a coordinated, guided, and supportive approach to simplifying and streamlining your healthcare experience.
Free Access to Concierge-Level Service
Your Health Resource Coordinator helps you navigate and get the most out of your Whole Health Plan benefits. They can help schedule appointments, address billing questions, and more!
Coordinated Care
Your Health Resource Coordinator is your point person across all care touchpoints, from your Primary Care Provider to your Health Coach and more.
Advocacy
Your Health Resource Coordinator is your advocate and will relay your concerns to the right people for a prompt resolution of concerns and questions.
To connect with a Health Resource Coordinator:
- Call 844-380-4554
- Email service.team@webtpa.com
- Use the chat or messages feature on your Member Portal
